By: Becky Spencer, PhD, APRN, PMHNP-BC, IBCLC, PMH-C, FILCA
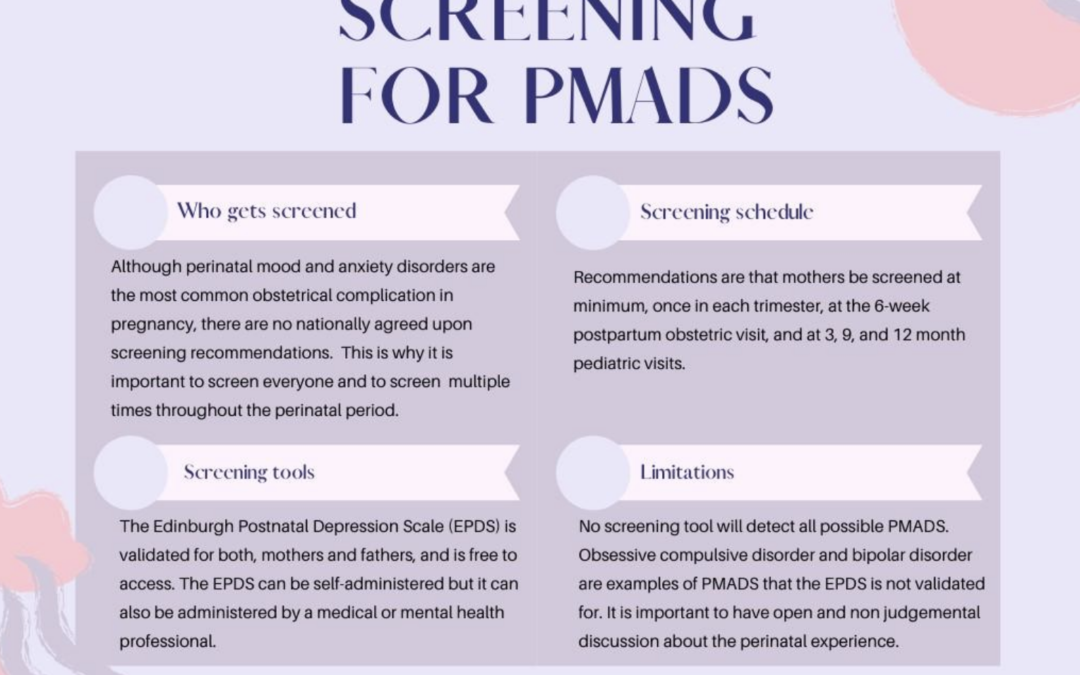
Getting diagnosed with a perinatal mood and anxiety disorder (PMAD) can be difficult. PMADs are the most common obstetrical complication in pregnancy, yet nationally agreed upon screening recommendations do not exist among professional medical organizations.
Other pregnancy complications like gestational hypertension and pre-eclampsia, which affect approximately 6-8% of pregnancies, are routinely screened for at every prenatal visit. Likewise, gestational diabetes, which affects approximately 6% of pregnancies, is routinely screened for after 24 weeks gestation.
PMADs affect up to 21% percent of women in pregnancy or during the first year postpartum (Wisner et al., 2013). Without consistent and routine screening, PMADs continue to be underdiagnosed and undertreated, and the actual number of people experiencing PMADs could be much larger.
Postpartum Support International, an organization that promotes awareness, prevention, and treatment of PMADs, recommends the following screening schedule:
- At the first prenatal obstetrical appointment
- At least once in the second trimester
- At least once in the third trimester
- At the 6-week postpartum obstetrical appointment
- At obstetrical or primary care appointments at 6-months and 12-months postpartum
- At 3, 9, and 12-month pediatric visits.
Valid and reliable screening tools for PMADs are widely available, free to access, and are quick to complete and evaluate. The Edinburgh Postnatal Depression Scale (EPDS) is validated for screening for PMADs for both mothers and fathers and can be self-administered.
The EPDS includes 10 screening questions total and includes specific questions for depression, anxiety, and suicide. Scoring of the EPDS and recommendations for action are as follows:
Score less than 8
- Depression not likely
- Continue support and follow-up screening
Score 9-11
- Depression is possible
- Re-screen in 2-4 weeks, consider referral to a provider who specializes in perinatal mental health
Score 12-13
- Fairly high possibility of depression
- Refer to a mental health provider who specializes in perinatal mental health
Score 14 and higher
- Probable depression
- Refer to a mental health provider who specializes in perinatal mental health
Positive score (1-3) on question 10
- Suicidal ideation or intent is possible
- Direct and immediate referral for a mental health crisis assessment at an emergency room, behavioral health hospital, or mental health crisis assessment center
Up to 10% of fathers experience PMADs and scoring guidelines for fathers for PMADs is suggested to be 2 points lower than cut-of scores for mothers listed above (Edmondson et al., 2010).
If a medical professional (obstetrician, pediatrician, midwife, or nurse practitioner for example) administers the EPDS with a patient and the score is 9 or more, the patient should be referred to a mental health care provider who has experience in treating PMADS. Postpartum Support International has a list of mental health care providers across the US that are specialized in treating PMADs.
Mental health conditions are the number 1 preventable cause of maternal mortality, with suicide being the most preventable cause. If a loved one who is pregnant or postpartum scores positive on question 10 of the EPDS or shares any thoughts about suicide take them seriously and get them help immediately. The most concerning statement from a loved one who is pregnant or postpartum is, “My baby would be better off without me.”
Help is available 24 hours a day from these National resources:
- National Crisis Text Line: Text HOME to 741741 from anywhere in the USA, anytime, about any type of crisis.
- National Suicide Prevention Hotline & Website: 1-800-273-8255
- www.suicidepreventionlifeline.org
The 5 most helpful things you can do and say to someone who is experiencing suicidal thoughts is:
- Ask them if they are having thoughts about suicide
- Listen without judgment and tell them that you care
- Remove any means for harm if it is safe and you are able
- Help them connect to resources for help
- Follow-up with a call or visit to see how someone is doing after you have provided help Asking for and receiving help is not a weakness.
Know that:
Asking for and receiving help is a strength.
Help is available and mental wellness is achievable.
References
BC Reproductive Mental Health Program and Perinatal Services BC. (2014), Best practice guidelines for mental health disorders in the perinatal period. http://www.perinatalservicesbc.ca/health-professionals/guidelines- standards/maternal
Cox JL, Holden JM, Sagovsky R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150(6), 782-786. https://doi.org/10.1192/bjp.150.6.782
Edmondson, O. J., Psychogiou, L., Vlachos, H., Netsi, E., & Ramchandani, P. G. (2010). Depression in fathers in the postnatal period: assessment of the Edinburgh Postnatal Depression Scale as a screening measure. Journal of Affective Disorders, 125(1-3), 365-368. https://doi.org/10.1016/j.jad.2010.01.069
Wisner, K. L., Sit, D. K., McShea, M. C., Rizzo, D. M., Zoretich, R. A., Hughes, C. L., … & Hanusa, B. H. (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry, 70(5), 490-498. https://doi.org/10.3410/f.718030385.793480195